General Description
Entamoeba histolytica is an ameba that feeds on cells in the human colon. It is the cause of amebic dysentery (bloody diarrhea) as well as colonic ulcerations. The infection is also referred to as amebiasis. If the organisms spread throughout the body via the bloodstream they may cause abscesses in the liver or, less frequently, other organs.
Morphology
The organism has two forms.
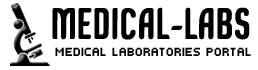
The trophozoite is 10 to 60 µm in diameter, ameboid, actively motile, and often erythrophagocytic. In stained specimens, the nucleus has a central karyosome with finely beaded peripheral chromatin.
The Cyst form
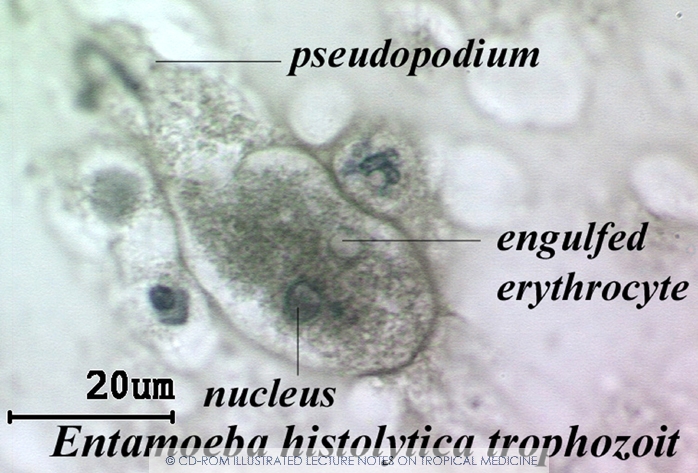
Encystation begins with the trophozoites become more spherical and the appearance of chromatoid bodies in the cytoplasm. Chromatoid bodies (cb) are stained elongated structures with round ends and represent the aggregation of ribosomes. The cyst wall is composed of chitin and has a smooth refractile appearance. Cyst maturation involves two rounds of nuclear replicationwithout cell division and cysts with 1-4 nuclei (Nu) are found in feces. Sometimes the young cysts (ie, 1-2 nuclei) will have a glycogen vacuole (vac) which will appear as a clear area in stained specimens. This vacuole will sometimes displace and alter the morphology of the nuclei. The chromatoid bodies tend to disappear as the cyst matures. The cysts are generally 12-15 µm in diameter. Cysts are immediately infective upon excretion with the feces and will be viable for weeks-to-months depending on environmental conditions.
Transmission
E. histolytica is spread by the fecal-oral route. This is achieved through food or water contaminated with cysts, oral-anal sexual contact, or occasionally directly in childcare centers or institutions for the developmentally challenged. The disease is found far more frequently in people from developing countries or travelers to such areas than in developed countries.
Pathogenesis & Clinical Manifestations
Pathogenic and non-pathogenic strains of E histolytica inhabit the human digestive tract. Even pathogenic strains may live in the lumen as benign commensals.
If mucosal invasion occurs, it may be limited to a few simple superficial erosions or it may progress to total involvement of the colonic mucosa with ulceration. The clinical manifestations vary with the extent of involvement. Mucosal erosion causes diarrhea, which increases in severity with increasing area and depth of involvement.
Symptoms are also affected by the site of the infection. The more distal the lesion in the colon, the greater the likelihood and severity of symptoms; thus small rectal lesions are more likely to be symptomatic than larger cecal lesions.
Rectal bleeding is only slightly less common than diarrhea and is usually, but not invariably, associated with diarrhea. Such bleeding may be grossly apparent or may be occult and demonstrable only by chemical testing for blood. Urgency, tenesmus, cramping abdominal pain and tenderness may be present.
Amebic dysentery has a dramatically different clinical presentation. The diarrhea is replaced by dysenteric stools consisting largely of pus and blood without feces. There is evidence of systemic toxicity with fever, dehydration, and electrolyte abnormalities. Tenesmus and abdominal tenderness are regular features. This fulminant presentation may occur suddenly or evolve from less severe, pre-existing disease.
Occasionally, and for no apparent reason, colonic infection with E histolytica will evoke a proliferative granulomatous response at an ulcer site. This infectious pseudotumor, called an ameboma, may become the leading point of an intussusception or may cause intestinal obstruction. This complication is uncommon.
Extraintestinal amebiasis begins with hepatic involvement. Many patients with acute intestinal infection also have hepatomegaly, but in these cases amebas are not demonstrable in the liver and the pathogenesis of this hepatomegaly is not clear.
A focal amebic abscess in the liver represents metastasis from intestinal infection. Symptomatic intestinal infection need not be present. The abscess appears as a slowly enlarging liver mass. Often the patient will have right upper quadrant pain, which may be referred to the right shoulder. If the abscess is located in a palpable portion of the liver, the area will be tender.
Occasionally the enlarging abscess presses on the common bile duct and causes jaundice. If located under the dome of the diaphragm, the abscess may cause elevation of the dome of the diaphragm which presses on the right lung base, causing atelectasis and physical findings of consolidation. As the abscess nears the diaphragm the inflammation may stimulate pleural effusion.
Pleural, pulmonary, and pericardial infection occurs as a result of direct extension from the liver. Lung involvement is far more common than pericardial infection. Infection metastatic from the liver can involve other viscera or can give rise to a brain abscess. However, these complications are uncommon
Diagnosis
Microscopic techniques employed in a diagnostic clinical laboratory include wet preparation, concentration, and permanently stained smears for the identification of E. histolytica in feces.
Microscopic examination of a direct saline (wet) mount is a very insensitive method which is performed on a fresh specimen.
The sample should be examined within 1 h of collection to search for motile trophozoites which may contain RBCs. However, in patients who do not present with acute dysentery, trophozoites will not contain RBCs.
Patients with asymptomatic carriage generally have only cysts in the fecal sample. Although the concentration technique is helpful in demonstrating cysts, the use of permanently stained smears (trichrome or iron hematoxylin) is an important method for recovery and identification of Entamoeba species.
As Entamoeba trophozoites generally degenerate rapidly in unfixed fecal specimens and refrigeration is not recommended, specimens should be preserved with a fixative which prevents the degradation of the morphology of the parasite and allows concentration and permanent smears to be performed.
Fixatives used for the concentration procedure include Schaudinn’s fluid, merthiolate iodine-formalin, sodium acetate-acetic acid-formalin (SAF), or 5% or 10% formalin. The fixatives for the permanently stained smears include trichrome, iron hematoxylin, Ziehl-Neelsen stains, modified polyvinyl alcohol (PVA) (containing mercury compounds), and SAF.
Culture Methods
Culture techniques for the isolation of Entamoeba species have been available for over 80 years. Culture media include xenic (diphasic and monophasic) and axenic systems. Xenic cultivation is defined as the growth of the parasite in the presence of an undefined flora Different monophasic media that were developed for E. histolytica are the egg yolk infusion medium of Balamus
Antibody detection methods
Many different assays have been developed for the detection of antibodies, including indirect hemagglutination (IHA), latex agglutination, immunoelectrophoresis, counterimmunoelectrophoresis (CIE), the amebic gel diffusion test, immunodiffusion, complement fixation, indirect immunofluorescence assay (IFA), and enzyme-linked immunosorbent assay (ELISA). A variety of antibody assays for detection of E. histolytica antibodies in human serum are also commercially available

Entamoeba histolytica/dispar. Formalin-fixed specimen. An immature cyst with two nuclei but without a vacuole.

Entamoeba histolytica. Amoebic dysentery. Wet mount examination (unfixed specimen). Numerous hematophagous trophozoites. The nucleus is never seen in this kind of preparation.
Entamoeba histolytica/dispar. SAF-fixed specimen, wet mount examination. Above, an elongated trophozoite with two nuclei (telophase). Below, a rounded one (pre-cystic form) with dot-like karyosome
treatment
Intestinal Infection: Usually nitromidazole derivatives are used because they are highly effective against the trophozoite form of the amoeba. Since they have little effect on amoeba cysts, usually this treatment is followed by an agent (such as paromomycin or diloxanide furoate) that acts on the organism in the lumen.
Liver abscess: In addition to targeting organisms in solid tissue, primarily with drugs like mitronidazole and chlorquine, treatment of liver abscess must include agents that act in the lumen of the intestine (as in the preceding paragraph) to avoid re-invasion. Surgical drainage is usually not necessary except when rupture is imminent.
Asymptomatic Patients: For asymptomatic patients (otherwise known as carriers, with no symptoms), non endemic areas should be treated by paromomycin, and other treatments includediloxanide furoate and iodoquinol. There have been problems with the use of iodoquinol and iodochlorhydroxyquin, so their use is not recommended. Diloxanide furoate can also be used by mildly symptomatic persons who are just passing cysts.
references :
web.uconn.edu
ncbi.nlm.nih.gov
atlas-protoza.com
wikipedia